Review: Acupuncture using pattern-identification appears to be effective in the treatment of insomnia
Kim, S. H., Jeong, J. H., Lim, J. H., & Kim, B. K. (2019). Acupuncture using pattern-identification for the treatment of insomnia disorder: a systematic review and meta-analysis of randomized controlled trials. Integrative medicine research, 8(3), 216–226.
https://doi.org/10.1016/j.imr.2019.08.002
QUESTION
Is acupuncture using pattern-identification effective in the treatment of insomnia?
DATA SOURCES
Randomized controlled trials (RCTs) were identified by searching PubMed, Cochrane CENTRAL, EMBASE, CINAHL, PsycINFO, CNKI, OASIS, NDSL, and RISS4U (from Jan 1, 2000 to April 12, 2018).
STUDY SELECTION
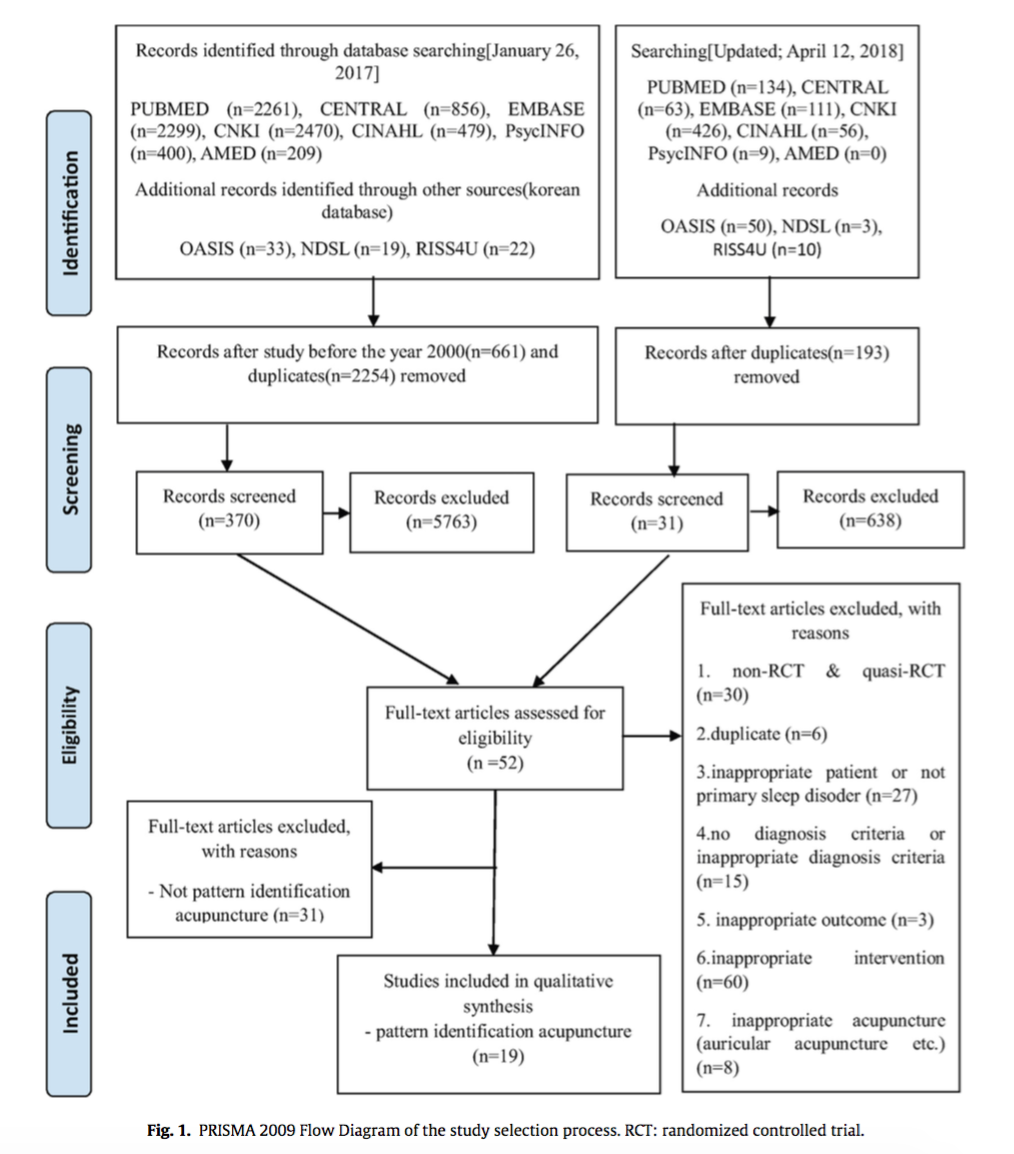
Randomized controlled trials (RCTs) that evaluate the effect of acupuncture and electroacupuncture, without regard to frequency or length of treatment, in patients diagnosed with primary insomnia were included (Fig 1).
DATA EXTRACTION
Two authors independently screened the studies and extracted data. Risk of bias evaluated using the Cochrane Collaboration’s risk of bias tool. Statistical analysis was performed using Review Manager version 5.3.
MAIN RESULTS
Meta-analysis showed that acupuncture significantly improved response rate and PSQI compared to medication.
CONCLUSION
Acupuncture using pattern-identification appears to be effective in the treatment of insomnia.
COMMENTARY
Authors identified 19 RCTs that address the question (Table 1). Sample size ranged from 25 to 192. Intervention in the treatment group of 11 studies was manual acupuncture and 8 studies was electroacupuncture. Interventions in the control group included medication, no treatment, and sham acupuncture. The primary outcome included response rate and Pittsburgh Sleep Quality Index (PSQI). Included studies were rated as low quality, overall risk of bias assessments were unclear or high, and publication bias was present.
Total of 16 pattern-identifications were used (3-7 pattern-identifications in each study). The most frequently used pattern-identification was “Deficiency of Heart and Spleen” (commonly used acupoints: SP-6, ST-36, BL-15, BL-20) and the most frequently used acupoints were GV-20, Si Shen Cong, An Mian, HT-7, and SP-6.
The result of 19 studies showed that the acupuncture group had a greater improvement in response rate than the medication group (Fig A). The result of the subgroup analysis showed that both acupuncture and electroacupuncture had a greater improvement in response rate than the medication group.
The result of 8 studies showed that the acupuncture group had a greater improvement in PSQI than the medication group (Fig B). The result of the subgroup analysis showed that both acupuncture and electroacupuncture had a greater improvement in PSQI than the medication group.
Authors conclude that “acupuncture using PI [pattern-identification] improved response rate and sleep quality compared with medication,” and suggest that, due to high risks of bias, clinical heterogeneity, and non-standardized pattern-diagnosis-criteria and acupoints, “further research comparing acupuncture using PI” is needed.